Diabetic retinopathy and maculopathy
Diabetic retinopathy is a complication of long-standing or poorly controlled diabetes. High blood sugar damages the small blood vessels in the retina (nerve layer) of the eye, causing patches of bleeding and leakage of proteins or fat within the retina.
There are several stages of retinopathy, and the transition from early stage to advanced retinopathy may take many years. This means that there are many opportunities for early and moderate stage retinopathy to be picked up before it reaches the later stages. Advanced retinopathy causes potentially blinding complications like severe bleeding, scar formation and retinal detachment.
Maculopathy (or diabetic macular edema) is a specific sub-type of diabetic retinopathy involving the central fixation point of the eye (macula). In these cases, the macula become swollen and vision may be affected early. Visual impairment may be permanent if not treated early.
Once retinopathy sets in, it indicates that significant damage has accumulated within blood vessels in the body, and it is possible that the kidneys, heart and small nerve endings of the fingers and toes have also been affected.
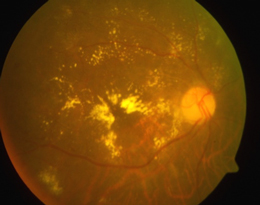
Diabetic maculopathy (macular edema).
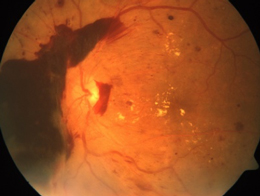
Advanced diabetic retinopathy with severe bleeding in the eye.
Treatment
In early stage diabetic retinopathy, eye treatments may not be necessary. However, good control of blood sugar levels will help to slow down the disease process and regular eye examinations are important to catch the disease if it enters a more severe stage.
More advanced stages of diabetic retinopathy and maculopathy may be treated in several ways:
Laser therapy is done to slow down the disease process and reduce the risk of visual loss. It is done as an outpatient procedure and may need to be performed over several sessions.

Laser treatment in progress.
Intravitreal “antiVEGF” injections are now considered standard treatment for many cases of diabetic maculopathy. This involves the injection of medication (antiVEGF agents) into the eye using a very tiny needle, and has been shown in clinical studies to deliver good vision results. The injection is done as an outpatient procedure and multiple injections may be necessary.
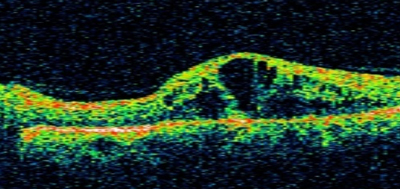
Eye scan shows a very swollen macula in diabetic maculopathy.
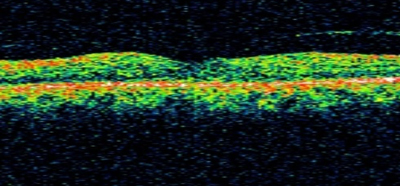
Eye scan shows resolution of the swelling after intravitreal injection therapy.
- Surgery
In very advanced retinopathy (proliferative diabetic retinopathy) where there is severe bleeding in the eye or a retinal detachment, “vitrectomy” surgery may need to be performed to remove the blood and scar tissue, or reattach the retina.
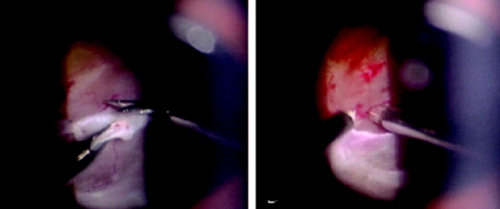
Micro-scissors and micro-forceps removing scar tissue during vitrectomy microsurgery.
Diabetic eye screening
All diabetics are recommended to undergo regular eye examinations to pick up diabetic retinopathy early. Even in the absence of symptoms, eye examinations should be done at least once a year as there may be no symptoms in early stages of retinopathy.
Those already diagnosed with diabetic retinopathy should be monitored more frequently for worsening which may require treatment.
The minimum eye screening will involve having a photograph taken of the retina (diabetic photoscreening). A detailed eye examination is recommended for those at higher risk of diabetic retinopathy or those not suitable for photoscreening. If diabetic retinopathy or maculopathy is seen, further tests like fluorescein angiography or “OCT” scans may be ordered to assess the extent of the damage.
FAQs about diabetic retinopathy and maculopathy
I am diabetic. How do I know if I am at risk of having diabetic retinopathy?
All diabetics are at risk of retinopathy, but the risks go up in those with unsatisfactory sugar control and those with longer duration (more than 5 years) of diabetes. The risk is also higher in individuals who have other medical conditions like hypertension and “high cholesterol” levels. If you are diabetic and pregnant, your risk will also go up. Eye screening is important if you have any of these risk factors.
I have early diabetic retinopathy but my doctor told me I require no treatment at this stage. Why have I not been given eyedrops or supplements to make me better?
No eye treatment is necessary for early diabetic retinopathy because the most effective treatment is good control of blood sugar levels with proper diet and diabetic medication. This will slow down the worsening of retinopathy, and may even reverse some early changes.
Eye treatments like laser, eye injections and surgery are usually recommended when retinopathy reaches specific stages when the benefits of treatment outweighs the risks of treatment. There are currently no eyedrops effective for diabetic retinopathy.
I have had laser done for diabetic retinopathy but why has vision not returned to normal?
Laser is usually done for advanced diabetic retinopathy. The objective is to limit visual loss or prevent blindness. Improvement in vision may not occur. In addition, by the time laser treatment is necessary, retinopathy is usually already in the advanced stage.
In such a case, improvement in vision is not expected due to the pre-existing irreversible damage. In individuals in whom vision is impaired by macular edema, intravitreal antiVEGF injections may be able to improve vision.
